COVID-19 Updates
– Updated: June 27th, 2022 –

COVID-19 Updates
To find an open and available COVID-19 vaccine clinic, please visit the Deschutes County webpage at https://www.deschutes.org/health/page/covid-19-vaccine
If you need an appointment for COVID-19 test, please schedule online with our Urgent Care clinic at https://www.clockwisemd.com/hospitals/2718/visits/new
Stay safe –
Your High Lakes Health Care Team
–
Facial Coverings Update
– Updated: March 3rd, 2022 –
Facial Coverings Are Still Required in Health Care Settings
When mask requirements are lifted for other indoor settings, you will still need to wear a mask in health care settings, following OAR 333-019-1011.
Masking is still required at all our health care facilities regardless of vaccination status or direct vs indirect patient contact. You must wear a mask. Why?
- It is an OHA policy for health care facilities (OAR 333-019-1011) and is enforced by Oregon OSHA.
- Breakthrough cases have and will continue to occur.
- Omicron variant spreads more easily than the Delta variant.
- We see many unvaccinated and/or immunocompromised patients.
FAQ
Here is a link to OHA’s Frequently Asked Questions.
https://sharedsystems.dhsoha.state.or.us/DHSForms/Served/le3898n.pdf
Thank you for your cooperation!
– Praxis Health Team
—
COVID-19 FAQ’s
Q. Who requires testing for COVID-19?
- If you are ill with any COVID-19 symptoms or have been in close contact with anyone with COVID-19 infection, testing is recommended. Other common reasons for testing include pre/post travel and preoperative testing.
Q. When should I get tested for COVID-19?
- If you are symptomatic, viral testing should be conducted early on in your course of illness.
- If you have been exposed but are asymptomatic, testing should be conducted 3-5 days after your exposure. This provides the best chance of early detection.
Q. How is close contact defined?
- Per Centers for Disease Control and Prevention (CDC), close contact is defined as being within less than 6 feet of distance for a total of 15 minutes or more to an individual with laboratory confirmed or probable COVID-19. This time is cumulative over a 24 hour period.
Q. How do I get tested for COVID-19?
- Testing requires an order from a High Lakes provider.
- You will need either an office visit or video visit with a provider to discuss testing and obtain an order.
- High Lakes has specific times and processes to have your sample collected and tested.
- For pre-operative testing, you will likely be tested at one of the various St. Charles lab locations. You will receive further information about this from our resource team.
- For all other scheduled testing (travel, exposure, illness) your provider will help determine the best location and time for testing. A drive through clinic outside of High Lakes Urgent Care operates daily beginning at 5:30PM (M-F) / 2:30 PM (Sat/Sun). Use of this service requires an order from your provider.
- Additional testing options can be arranged on a case by case basis.
- To arrange an appointment with your provider, you can call High Lakes or send a portal message
- To arrange an appointment with urgent care, you can schedule online at highlakeshealthcare.com or call the urgent care directly.
Q. What test do I need? (Your provider will decide this with you)
- To determine if you have active COVID-19 infection, a viral test is needed. Test options include:
- PCR– this is the most sensitive test and is performed by an outside lab. High Lakes uses Interpath Lab for this test. Specimen collection is usually via nasal swab. Results are typically returned in 1-4 days.
- Rapid molecular testing– High Lakes Urgent Care uses the Abbott ID Now test kit. Samples are collected via nasal swab and tested on-site. Test results are available within 15 minutes. This test is best for symptomatic patients requiring immediate results although there are other acceptable indications.
- Rapid antigen testing– This test is also run on site using a nasal swab. Similar to the rapid molecular test, this test performs best in symptomatic patients requiring immediate results. High Lakes uses the Abbott BinaxNow test. This test is less sensitive before symptoms begin.
Q. What is an antibody test?
- An antibody test attempts to detect circulating COVID-19 antibodies in your system. This requires a blood draw and is generally performed at least 1-3 weeks after illness. This test can be helpful to support a diagnosis of COVID-19, but should not be used to diagnose an active infection or determine immune status to COVID-19.
Q. What do I do while awaiting test results?
- You will be asked to quarantine until your results are known. Quarantine duration will depend on several factors, including symptoms, exposure, reason for testing and test results.
Q. Will High Lakes offer the vaccination when it becomes available?
- High Lakes is currently offering the Moderna vaccine. More information is available on the High Lakes website, COVID-19 section (http://highlakeshealthcare.com/covid-19/).
Q. If I have symptoms of illness or exposure can I still see my provider for a routine visit?
- For all patients who have illness or exposure, we are asking on-site visits be changed to video visits, if appropriate. If an on-site visit is required, the care team will help determine the best location and safest way to provide care for your condition.
- High Lakes Primary Care and Urgent Care will continue to be available to address your same day needs.
Patient asking for advice after testing positive for COVID:
Q. I have tested positive for COVID. Do you have any advice for me?
- We know having COVID-19 can feel scary and isolating. The team at Praxis Health/High Lakes Health Care is here to support you. The following is meant as a guide for you during this time. Please do not hesitate to call, portal or schedule an appointment if you need further assistance.
- Stay home except to get medical care. Most people with COVID-19 have mild illness and can recover at home without medical care. Do not leave your home, except to get medical care. Alert medical offices of your diagnosis and symptoms so they can see you in the safest environment for you, other patients and staff. Do not visit public areas.
- Separate yourself from other people: As much as possible, stay in a specific room and away from other people and pets in your home. Use separate bathroom if possible.
- Get rest and stay hydrated. Take over the counter medicines, such as acetaminophen, to help you feel better.
- Seek emergency medical attention if:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion
- Inability to wake or stay awake
- Bluish lips or face
https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/steps-when-sick.html/
https://multco.us/novel-coronavirus-covid-19/covid-19-after-you-get-tested
Q. What treatments are available locally?
- St. Charles is offering monoclonal antibody treatment to qualifying COVID-19 positive patients.
- Providers will help determine who qualifies.
- The specific treatment is REGEN-COV (casirivimab and imdevimab) and must be prescribed by a provider. Patients cannot self-refer for this treatment.
Patients Inquiring about COVID-19 Vaccine
Q. Are you able to determine when I will receive the COVID-19 vaccine?
- As of now, everyone 12 or older is eligible for the COVID-19 vaccine. Patients can currently register for a COVID-19 vaccine by visiting www.centraloregoncovidvaccine.com.
Q. Is the COVID-19 vaccine safe?
- COVID-19 vaccines were tested in large clinical trials to make sure they meet safety standards. Many people were recruited to participate in these trials to see how the vaccines offers protection to people of different ages, races, and ethnicities, as well as those with different medical conditions.
- The Pfizer vaccine has recently received full FDA approval. The FDA and CDC will continue to monitor the safety of COVID-19 vaccines, to make sure even very rare side effects are identified.
Q. Can I get on a wait list?
- HLHC will be notifying patients of vaccine distribution when we have more information. We will not be developing a wait list.
Q. How can I stay informed on vaccine information from High Lakes?
- Please ensure you have signed up for the patient portal and provided High Lakes a valid email address. Also follow us on social media. We will likely use multiple outlets to keep patients informed.
- The CDC is also an excellent resource for vaccine information: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/8-things.html
Q. I was recently diagnosed with COVID-19 and am scheduled to receive the vaccine. How long do I need to wait?
- Per the CDC, it is recommended you still receive the vaccine. You can receive the vaccine as soon as you have completed the quarantine requirements for your condition.
- For most individuals this will be after 10 days from symptom onset and at least 24 hours since last fever and other symptoms have improved.
- For patients hospitalized or who are severely immunocompromised, the period is extended to at least 20 days from symptom onset, along with improvement in symptoms and fever free for at least 24 hours.
- One other exception is anyone who has received monoclonal antibody treatment. These individuals must wait 90 days from treatment.
Resource https://www.cdc.gov/vaccines/covid-19/info-by-product/clinical-considerations.html
Q. I have received the COVID-19 Vaccine, do I need a booster shot?
- Under current conditions, the FDA is recommending an additional dose of vaccine for those thought to have an inadequate immune response to primary vaccine series. Booster doses are expected to be approved for the remaining population this fall but have not been approved to date. The following is a list of conditions that qualify for an additional dose under current guidelines:
- Are undergoing active treatment for solid tumor and hematologic malignancies
- Have received solid-organ transplant and are taking immunosuppressive therapy
- Have received CAR (chimeric antigen receptor)-T-cell or hematopoietic stem cell transplant (within two years of transplantation or are taking immunosuppression therapy)
- Have moderate or severe primary immunodeficiency (e.g., DiGeorge, Wiskott-Aldrich syndromes)
- Have advanced or untreated HIV infection
- Are undergoing active treatment with high-dose corticosteroids (i.e., ≥20mg prednisone or equivalent per day), alkylating agents, antimetabolites, transplant-related immunosuppressive drugs, cancer chemotherapeutic agents classified as severely immunosuppressive, TNF blockers, and other biologic agents that are immunosuppressive or immunomodulatory
- Stem cell transplant within the last two years
- For qualifying patients, the additional dose must be administered at least four weeks after a second dose of mRNA (Pfizer or Moderna) COVID-19 vaccine. Efforts should be made to receive the same vaccine with the third dose as received with the initial two doses. If the mRNA vaccine product given for the first two doses is not available or is unknown, either mRNA COVID-19 vaccine product may be administered.
Q. What about additional doses or booster doses for J&J vaccine recipients?
- This is not currently recommended as there is not enough data to determine if an additional dose or booster dose would improve antibody response.
Q. I received the Johnson and Johnson vaccine, do I need to worry about blood clots or Guillain-Barre Syndrome?
- For clotting disorders
- There have been rare cases of clotting disorders associated with the Johnson & Johnson (J&J) vaccine- approximately one case per one million administered doses. All cases occurred among women aged 18–48 years. The interval from vaccine receipt to symptom onset ranged from 6–13 days.
- The delivery of this medication was temporarily paused to investigate, but has now been authorized to resume delivery.
- If you develop severe headache, abdominal pain, leg pain, or shortness of breath, please contact your provider. It is important to let them know when you received the J&J vaccine.
- For GBS
- The CDC has reported a small risk of developing GBS (100 cases in 12.8 million doses) following receipt of the J&J vaccine
- Most cases were reported about two weeks after vaccination and mostly in males with risk lasting for 42 days following vaccination.
- GBS is a rare condition that damages nerve cells. Most recover but some have had permanent nerve damage.
- It has also been associated with flu vaccine although GBS is more common to occur after contracting influenza vs receiving the influenza vaccine.
Q. I was recently diagnosed with COVID-19 and am scheduled to receive the vaccine. How long do I need to wait?
- Per the CDC, it is recommended you still receive the vaccine. You can receive the vaccine as soon as you have completed the quarantine requirements for your condition.
- For most individuals this will be after 10 days from symptom onset and at least 24 hours since last fever and other symptoms have improved.
- For patients hospitalized or who are severely immunocompromised, the period is extended to at least 20 days from symptom onset, along with improvement in symptoms and fever free for at least 24 hours.
- One other exception is anyone who has received monoclonal antibody treatment. These individuals must wait 90 days from treatment.
Resource https://www.cdc.gov/vaccines/covid-19/info-by-product/clinical-considerations.html
Q. Should I get an antibody test to determine if the COVID-19 vaccine was effective?
- No- the antibody test is not designed for this purpose.
- Some people who have received the COVID-19 vaccine will still test negative for antibodies.
- A negative antibody test does not mean the vaccine is ineffective, rather the antibody test is designed to check for different antibodies.
- Similarly, a positive antibody test does not guarantee immunity.
Q. Can I be tested for the COVID-19 Delta variant?
- This test is performed by the state lab and requires approval.
- Currently this test is reserved only for patients being treated in the hospital setting.
Q. I am fully vaccinated but have been exposed to COVID-19. What are the recommendations?
- Get tested 3-5 days following a known exposure to someone with suspected or confirmed COVID-19 and wear a mask in public indoor settings for 14 days after exposure or until a negative test result.
- Get tested if experiencing COVID-19 symptoms.
|
– Updated: March 8, 2021 –
Patients who received their first vaccine dose with us on February 10, 11, & 16 will still be able to receive their second dose with us on March 10, 11 and 16. Your March appointment date and time was written for you on your vaccine card that you received after your shot.
Our team will also be making calls to confirm your second dose appointment date and time. The second dose appointments will be held at the same location as your first dose – High Lakes Upper Mill 929 SW Simpson Avenue, Suite 210 Bend, OR 97702.
For patients looking forward to their first dose…
Oregon Health Authority allocated 2,340 first-dose COVID-19 vaccines to Deschutes County for the week of March 1. All of those doses were administered at the St. Charles Vaccination Clinic at the Deschutes County Fairgrounds with recipients having made through this link. News reports show that the relatively small number of appointments filled up in less than an hour.
As of Monday, March 1, Deschutes County residents age 65 and older will be eligible to receive the vaccine. As soon as we have confirmation from the state that High Lakes Health Care will receive a vaccine supply, we will send an email like this, and will update our Facebook and Instagram pages. Please like and follow our social media pages so you have the latest High Lakes information as quickly as possible.
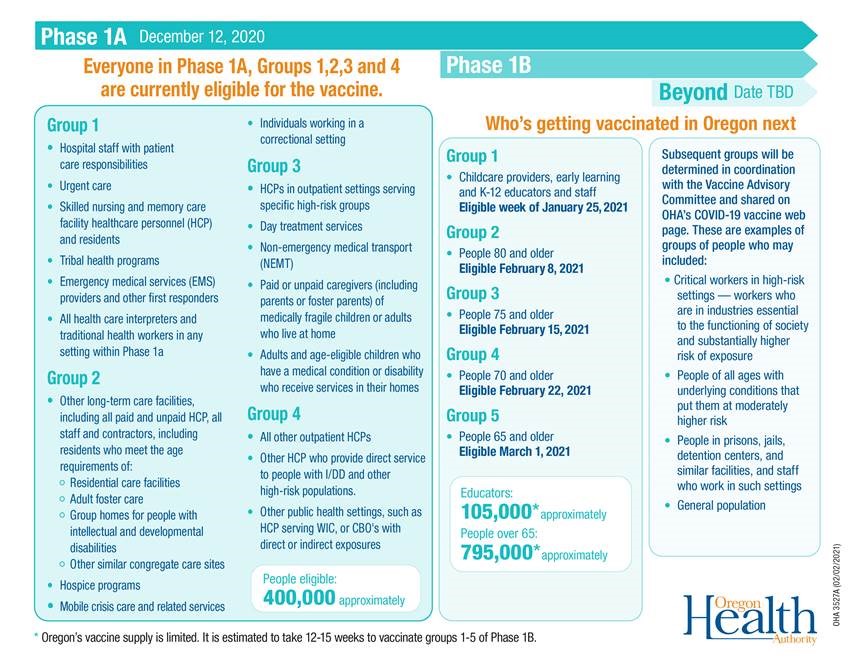
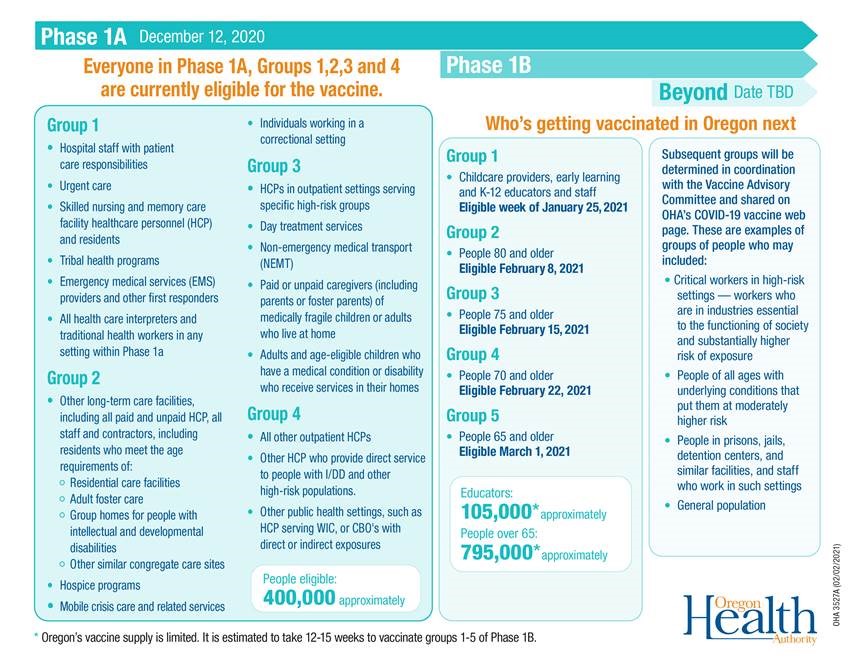
On March 1, Governor Brown announced the upcoming vaccine sequencing phases. Phase 1B, Group 6 will include adults 45–64 with one or more underlying health conditions with increased risk, migrant and seasonal farm workers, seafood and agricultural workers, food processing workers and people living in low-income senior housing, senior congregate and independent living. This group will become eligible to receive the vaccine beginning March 29. |
To learn more about the COVID-19 vaccine in Central Oregon
Visit:
We are following the Oregon Health Authority phased guidance regarding which groups are eligible for the vaccine, and when.
We will continue to update our patients on a weekly basis, regarding which groups we are open to scheduling vaccine appointments for.
Oregon Health Authority
Centers for Disease Control
World Health Organization